I probably came across this diagnosis early in my pathology training, but I didn’t pay much attention to it because nobody was talking about it—apparently, there wasn’t much interest in this entity.
Books state that nodular fasciitis is relatively frequent, but to be perfectly honest, I don’t think so. Let’s dive into it.
What is it?
A benign, self-limited fibroblastic proliferation (yes, a neoplasm—I know, the name doesn’t sound like one).
Variants
- May arise in association with vessels (intravascular fasciitis) or on the scalp of infants (here’s an example: link).
- Can present at a wide range of ages.
- Most common sites: subcutaneous tissue of the extremities, trunk, head, and neck.
- Usually small and non-tender.
- Rapid growth.
Treatment
Conservative excision. Prognosis is good, and recurrences are rare.
Pathology (to the point)
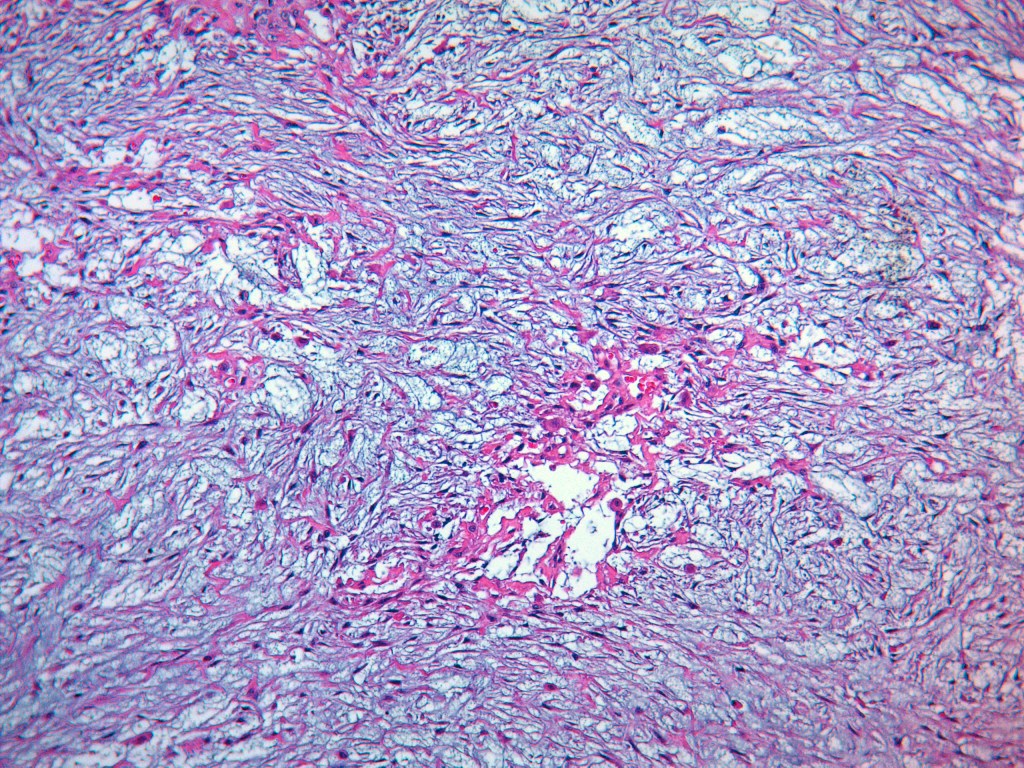
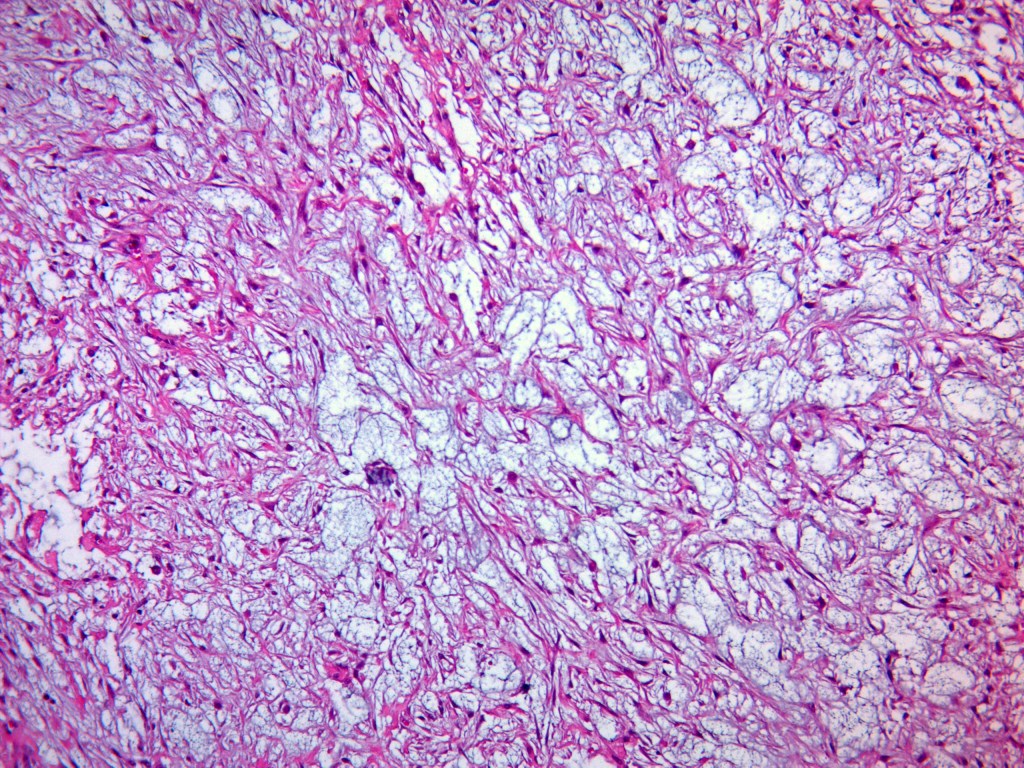
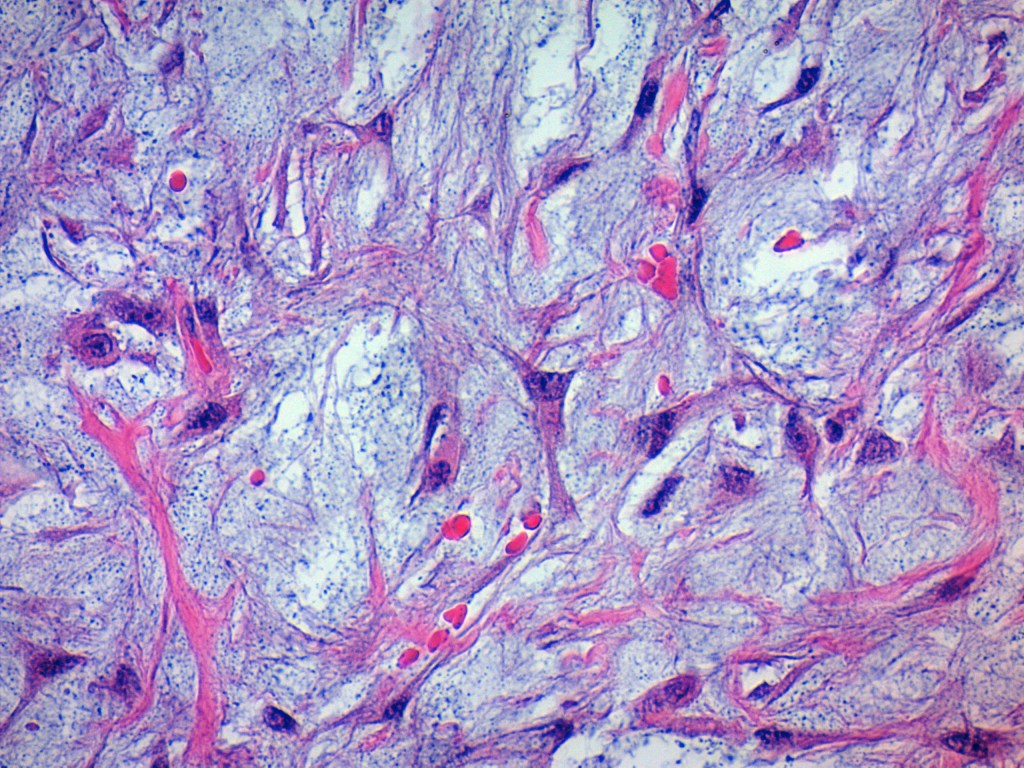
- Well-circumscribed but unencapsulated.
- Borders are well demarcated but may show focal infiltration.
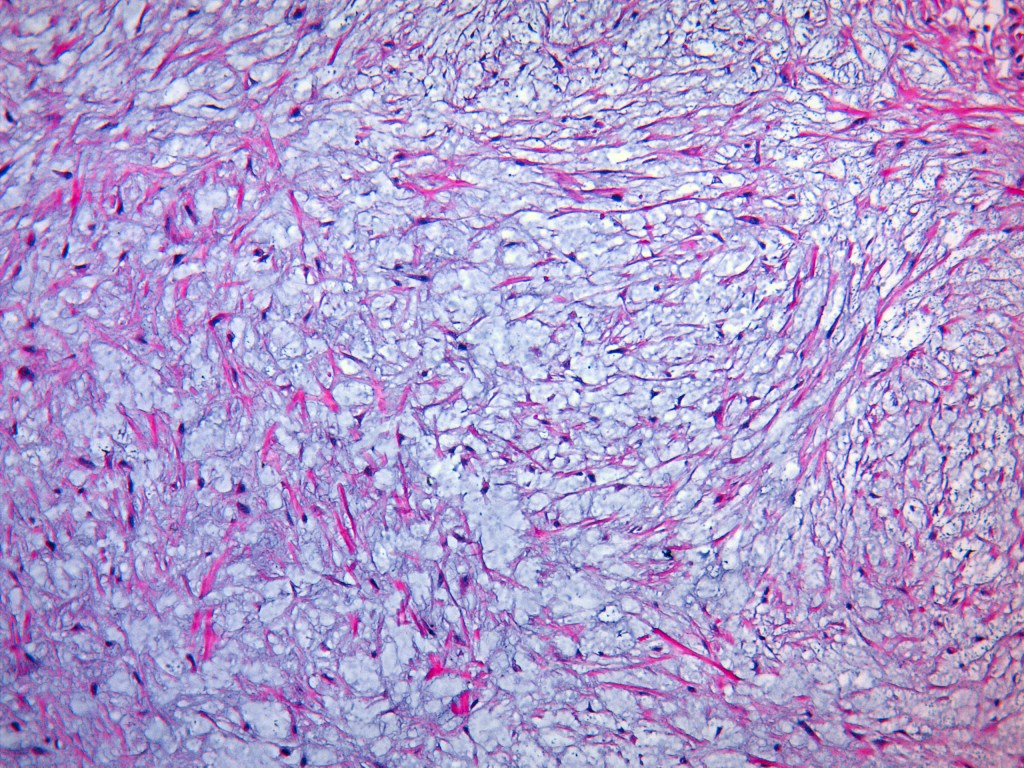
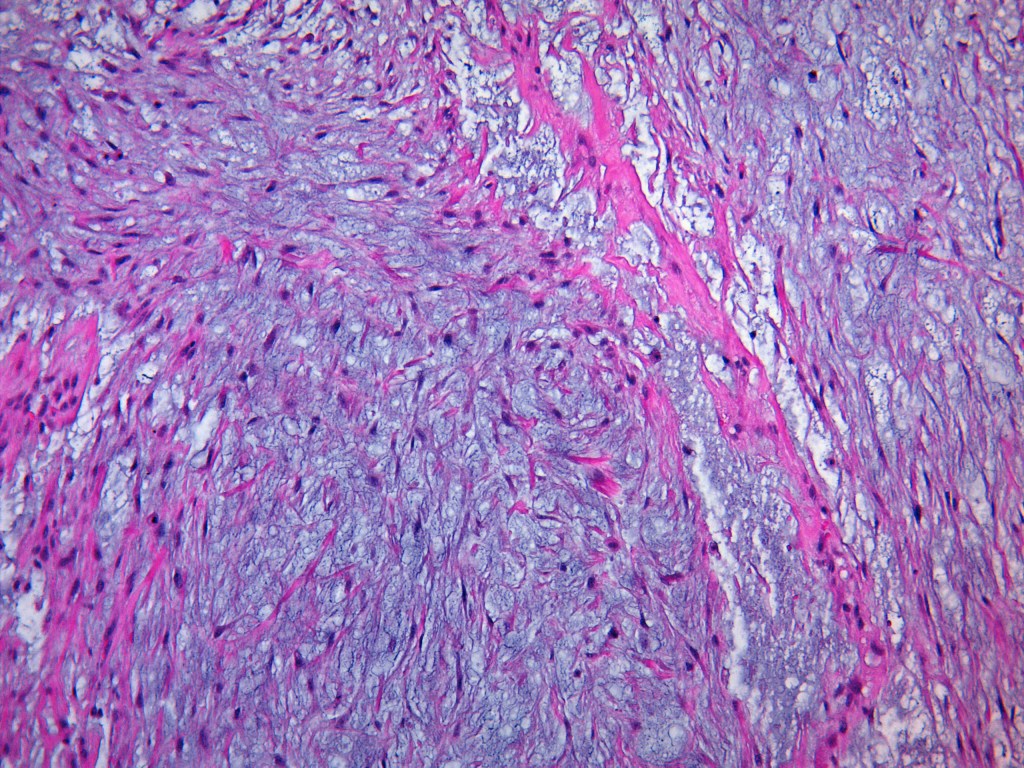
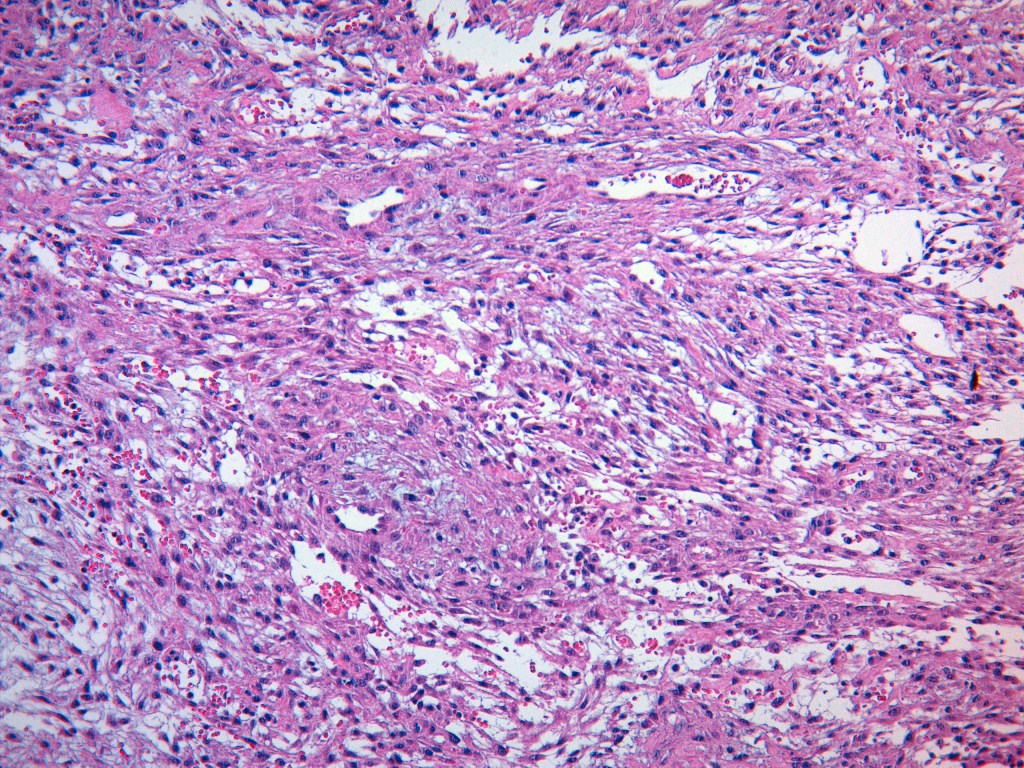
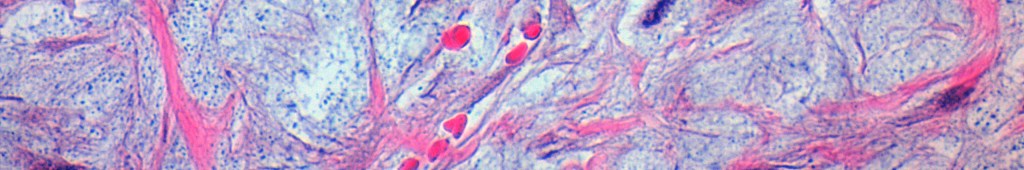
- Composed of plump fibroblasts with eosinophilic cytoplasm, arranged in a short fascicular pattern.
- Resembles fibroblasts in cell culture (here’s an example: link).
- Mitoses can be numerous.
- Abundant loose to myxoid stroma.
- Occasional thick, «keloidal» type collagen.
- Extravasated erythrocytes.
- Histiocytes.
- A few osteoclast-type giant cells—just because.
Immunohistochemistry
- SMA: diffusely positive (most useful marker).
- Negative for: Keratin, S100, CD34, and nuclear β-catenin (though IHC is not necessary in an otherwise typical case).
Differential Diagnosis
The list is long and often depends on the anatomic site and the specialty of the pathologist on the other side of the scope. Just to mention a few:
- Fibromatosis
- Myofibroma
- Neurofibroma
- Myxoid peripheral nerve sheath tumor
See you next time (note to self).

Deja un comentario